Common Reasons for Medical Billing Denials and How to Avoid Them


Common Reasons for Medical Billing Denials and How to Avoid Them
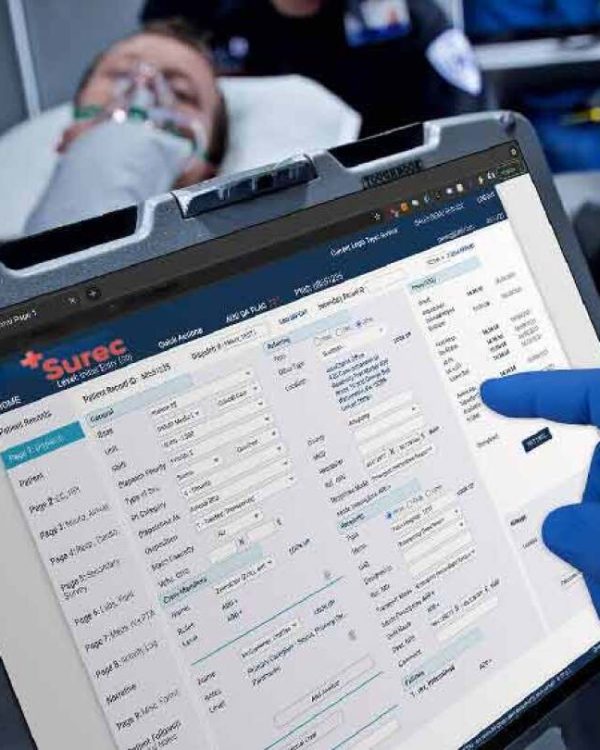
Medical billing denials are a significant obstacle to maintaining a healthy revenue cycle for healthcare providers. Understanding why claims are denied and taking proactive steps to avoid common mistakes can save time, reduce stress, and improve your financial outcomes. At Paramedic Billing Services, we are committed to helping you minimize denials through education and expert support. Here, we outline the most frequent reasons for medical billing denials and provide tips on how to avoid them.
1. Incorrect or Incomplete Patient Information
One of the most common reasons for claim denials is incorrect or incomplete patient information. Something as simple as a misspelled name, wrong date of birth, or missing insurance ID number can lead to an automatic denial. This type of error can often be avoided by double-checking patient data during registration and verifying the information before claim submission.
How to avoid:
- Verify patient demographics during each visit.
- Ensure that insurance information is up-to-date.
- Double-check all details before submitting the claim.

2. Insurance Coverage Issues
Another major cause of denied claims is related to insurance coverage. Claims may be denied if the patient’s insurance plan doesn’t cover the service provided, or if coverage lapsed prior to the date of service. It’s also common for denials to occur when services require prior authorization, and the authorization was not obtained before the treatment was rendered.
How to avoid:
- Confirm coverage eligibility before providing services.
- Obtain prior authorizations when required by the insurer.
- Review the patient’s insurance plan for any changes in coverage.
3. Inaccurate Coding
Incorrect or incomplete coding is a frequent source of denials. Medical codes must accurately reflect the services provided, and even minor errors in coding can lead to claim rejections. This includes using outdated codes, undercoding, or miscoding the procedure entirely. Ensuring that billing and coding staff are well-trained and up-to-date on coding standards is critical to reducing errors.
How to avoid:
- Provide regular training on the latest coding updates.
- Implement a review process to catch coding errors before claim submission.
- Utilize coding software to assist with accuracy.


4. Missing or Late Claim Submission
Timeliness is crucial when submitting claims. Insurance companies have strict deadlines for when a claim must be filed. Missing the deadline often results in the claim being denied. Additionally, claims may be denied if key documentation, such as medical records or supporting documentation, is missing.
How to avoid:
- Submit claims as soon as possible after services are rendered.
- Track submission deadlines for each payer.
- Ensure all required documentation is included with the claim.
5. Lack of Medical Necessity
Insurers may deny claims if they believe that the treatment provided was not medically necessary based on the patient’s condition or the payer’s guidelines. This type of denial can often be avoided by providing comprehensive documentation that justifies the treatment.
How to avoid:
- Ensure detailed and accurate documentation of the patient’s condition and treatment rationale.
- Clearly communicate with patients about coverage limitations before treatment.
- Stay informed about insurer guidelines regarding medical necessity.


Best Practices for Avoiding Denials
While claim denials are sometimes unavoidable, taking proactive measures can significantly reduce the likelihood of denials and streamline the billing process. At Paramedic Billing Services, we focus on implementing best practices to help you avoid these costly disruptions to your revenue cycle.
Best practices include:
- Thorough training: Keep your billing staff up-to-date with the latest coding and billing guidelines.
- Eligibility checks: Perform insurance verification before every patient visit.
- Pre-authorization management: Ensure you obtain necessary pre-authorizations in advance.
- Regular audits: Conduct regular audits of submitted claims to catch errors early.
- Follow-up: Establish a system for tracking and following up on claims to resolve issues quickly.
Why Use Paramedic Billing Services
Handling medical billing denials requires a skilled and dedicated team, and at Paramedic Billing Services, we provide the expertise needed to minimize errors and denials. Our thorough approach to billing ensures that common issues like coding errors, incomplete information, and missed deadlines are addressed before they become a problem. By partnering with us, you can reduce the frustration and financial loss associated with denied claims, ensuring smoother revenue flow and more time for patient care.

